- The Nimitz Report
- Posts
- The Community Care Conundrum
The Community Care Conundrum
HVAC examined the shortcomings in VA care and debated whether community care is the solution during yesterday's hearing.
⚡NIMITZ NEWS FLASH⚡
“Right Time, Right Place, Right Treatment with VA Community Care”
House Veterans Affairs Committee, Health Subcommittee Hearing
July 15, 2025 (recording here)
HEARING INFORMATION
Witnesses & Written Testimony (linked):
Dr. Kyleanne Hunter: Chief Executive Officer, Iraq and Afghanistan Veterans of America
Ms. Kristina Keenan: Director of National Legislative Service, Veterans of Foreign Wars
Ms. Dallas Knight: Founder & President, Operation Juliet, Army Combat Veteran
Dr. Meaghan Mobbs: Director, Center for American Safety and Security. Independent Women’s Forum
Ms. Amanda Newman: Chief Executive Officer, Western Illinois Home Health Care
Keywords mentioned:
Community care, specialty care, VA MISSION Act, wait times, workforce challenges, mental health, community providers, electronic medical records, Medicaid cuts, rural access, patient outcomes, training standards, coordination issues, legislative reform
IN THEIR WORDS
“Neither my husband nor I desire to receive care at the VA hospital... We’re asking for the same choice for all veterans.”
“We will get to a point... where a veteran will only have one choice, and that will be to go to the community for their care.”
“Veterans don’t need more bureaucracy, they need choice, they need speed, and they need a system built to serve them, not the other way around.”
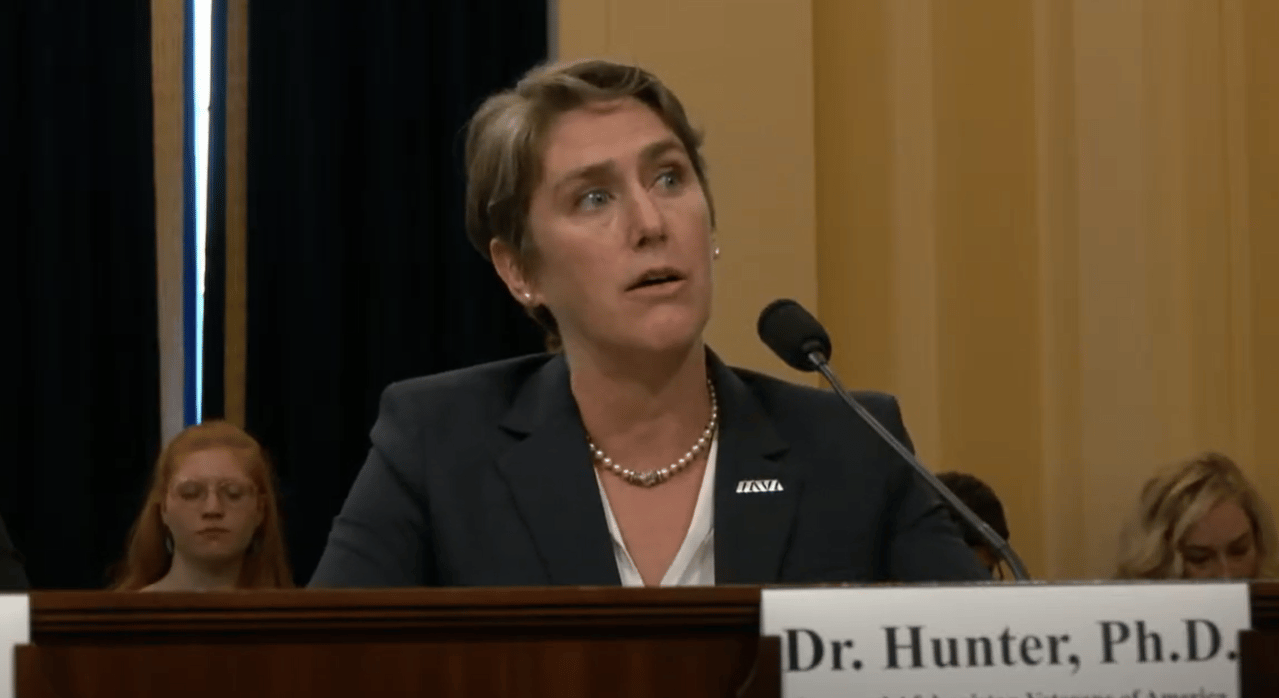
Dr. Kyleanne Hunter was one of several panelists who spoke in support of community care.
OPENING STATEMENTS FROM THE SUBCOMMITTEE
Chairwoman Mariannette Miller-Meeks mentioned the importance of the VA’s Community Care Program (VCCP) in meeting veterans’ specialty care needs. She stated that veterans benefit from community care through shorter wait and drive times, which is critical as the demand for specialty care increases. She highlighted the national healthcare workforce shortage impacting both the VA and private sector and noted regional shifts in care demands, especially for mental health. The Chairwoman claimed that the VA cannot meet veterans' needs with in-house care alone and stressed the importance of community providers in delivering timely, quality care.
Ranking Member Julia Brownley criticized the Trump administration’s policies, citing hiring freezes, workforce reductions, and return-to-office mandates that have made the VA a less desirable place to work. She warned that nearly 30,000 VA employees are expected to leave by September, including essential frontline staff like nurses and mental health providers, which has already increased wait times for care. Ranking Member Brownley also expressed concern that the recently passed "big, beautiful betrayal bill" would exacerbate pressures on rural healthcare by cutting Medicaid. She argued that while community care is necessary, the administration’s chaotic policies undermine the VA’s internal capacity and risk worsening veterans’ healthcare access overall.
Following the Ranking Member’s opening statement, Chairwoman Miller-Meeks rebutted by pointing out that workforce attrition rates at the VA are consistent with prior administrations and that the VA's funding and staffing had significantly increased in recent years. She underlined that House Republicans and VA Secretary Doug Collins are committed to reforming the VA to better serve veterans. The Chairwoman insisted that poor-performing VA employees must be held accountable and reiterated her confidence in the Trump administration’s efforts to improve the system.
SUMMARY OF KEY POINTS
Ms. Dallas Knight shared her personal struggles with the VA healthcare system, particularly regarding mental health and military sexual trauma (MST). She described inadequate and insensitive treatment by undertrained VA providers and the difficulty in accessing trauma-informed care and community care options. Ms. Knight presented the story of a fellow veteran who died due to untreated PTSD and systemic failures, illustrating the tragic consequences of poor care coordination. She urged the Subcommittee to listen to the voices of hundreds of women veterans demanding a system that treats them with dignity and respect.
Dr. Meaghan Mobbs highlighted that the VCCP was created to prevent tragedies like the Phoenix VA scandal by providing veterans with timely and flexible care. She criticized bureaucratic obstacles that continue to delay veterans’ access to necessary treatment and underscored that community care currently provides nearly 40% of all VA care. Dr. Mobbs advocated for a system based on flexibility, accessibility, speed, and accountability, particularly for women and rural veterans. She stressed that the issue is not funding but the VA’s failure to adapt and decentralize to meet veterans where they are.
Ms. Amanda Newman testified that community care is a crucial extension of the VA, especially for rural veterans who face barriers to in-home services. She identified three key obstacles: reduced services, shortened authorization periods causing instability, and inadequate reimbursement rates for rural providers. Ms. Newman shared examples of veterans denied essential services like homemaker assistance and physical therapy, illustrating the real-world impact of these barriers. She called for strengthening community care through better coordination, fair reimbursement, and investments in home and rural care access.
Ms. Kristina Keenan acknowledged that community care is essential for specialized services the VA cannot provide, but she noted persistent coordination problems. She shared personal experiences of billing delays and poor record-sharing, including a painful incident where the VA mistakenly believed she had terminated a pregnancy. Ms. Keenan said that veterans often face confusion over referrals and scheduling due to inconsistent communication from the VA. She endorsed legislative solutions like the Veterans’ ACCESS Act (H.R. 740) to improve community care oversight and coordination while reaffirming that many veterans still prefer direct VA care.
Dr. Kyleanne Hunter argued that while community care is necessary in some cases, VA direct care generally produces better health outcomes and cost savings. She cited evidence showing lower mortality, reduced hospital readmissions, and a 25% lower suicide rate among veterans receiving VA direct mental health care versus community care. Dr. Hunter claimed that the VA is uniquely capable of coordinating complex care needs, particularly for post-9/11 veterans with multiple health conditions. She advocated for expanded VA services, particularly community-based outpatient clinics, while cautioning against overreliance on community care as a substitute for direct VA services.
Ranking Member Brownley asked Dr. Hunter to elaborate on why military cultural competency makes VA providers uniquely positioned to care for veterans. Dr. Hunter responded that VA providers undergo extensive training on military cultural competency, including awareness of compound exposures, mental and physical health interactions, and military-specific traumas. She shared a personal example where a VA optometrist identified her ocular melanoma linked to her service, which community providers had missed. Dr. Hunter said that while the MISSION Act requires community provider training, there is no oversight to ensure it occurs.
Ranking Member Brownley asked Dr. Hunter to clarify whether a RAND study cited by Dr. Mobbs claimed that VA providers lacked training. Dr. Hunter confirmed that she contributed to that RAND study and explained that while VA provider training was known, there was no oversight of training for community care providers.
The Ranking Member followed up about the data and what it indicates about veterans' care preferences and outcomes. Dr. Hunter stated that evidence overwhelmingly shows that veterans prefer VA care, which yields better outcomes. She cautioned against policymaking based solely on anecdotes, reiterating the importance of data showing VA care is superior in quality and coordination.
Ranking Member Brownley asked for suggestions on helping veterans and the public better understand the evidence supporting VA care. Dr. Hunter recommended that veterans service organizations (VSOs) play an educational role and that Congress engage with VA providers to ensure transparency and oversight on care quality.
Rep. Greg Murphy asked Dr. Hunter to clarify whether her ocular melanoma diagnosis was caught because of VA providers' military knowledge or because of their general competence. Dr. Hunter explained that a community optometrist had missed the diagnosis despite it being visible in prior imaging, but the VA provider, familiar with military exposures, caught it during a routine appointment. Rep. Murphy argued that the difference in diagnosis reflected provider skill rather than VA versus community care.
Rep. Murphy also questioned post-operative care outcomes and suggested that higher-risk and costlier surgeries are typically referred out, skewing comparisons. Dr. Hunter agreed to provide specific data for the record.
Rep. Murphy turned to Ms. Knight, asking whether community care improves her access to VA-covered healthcare. Ms. Knight responded that living in rural Montana, community care gave her options not available at the VA, such as chiropractic and acupuncture for migraines. She noted that her community provider proactively asked her preferences regarding provider gender, a sensitivity not often encountered in the VA system. Dr. Murphy concluded that both VA and community care offer good and bad experiences, and veterans should have more control and choice in selecting providers.
Rep. Kelly Morrison asked what the data says about improving timely, quality care at the VA. Dr. Hunter underlined the importance of investing in patient-centered care teams, which are too often deprioritized. She added that better coordination between community providers and VA care teams is essential to ensure comprehensive treatment plans and avoid repetitive, traumatic recounting of medical histories by veterans. Rep. Morrison agreed that while community care is necessary, Committee actions should not undermine the VA’s capacity for direct care and research.
Rep. Kimberlyn King-Hinds asked Dr. Mobbs to expand on her recommendation for a comprehensive metric system to improve community care oversight. Dr. Mobbs explained that the GAO has provided recommendations on improving oversight, particularly tracking scheduling performance and implementing meaningful accountability metrics. She cited the VA’s Referral Coordination Initiative as an example needing clearer guidance and better performance tracking.
Rep. King-Hinds then asked for suggestions to improve accountability and coordination in the community care program. Dr. Hunter suggested enhancing VA modernization efforts, specifically the electronic health record (EHR) system, to improve communication between VA and community providers. She also recommended establishing transparent, enforceable standards for community care providers on training and care coordination, noting that these standards are lacking despite being required by the MISSION Act.
Rep. Herb Conaway inquired about how the loss of rural hospitals, potentially exacerbated by Medicaid cuts, would impact veterans' access to care. Ms. Newman responded that in her rural area, hospital closures have already limited access to care. Although her home care agency is less directly impacted by Medicaid cuts, she mentioned that local residents are accustomed to traveling for care due to existing hospital losses. Rep. Conaway reflected that despite VA Secretary Collins’ prior assurances, Medicaid cuts are now occurring and will likely cause "devastating dislocation" in rural areas, further straining veteran care.
Rep. Sheila Cherfilus-McCormick asked for recommendations to bridge the communication gap between community care providers and VA offices, particularly regarding timely, standardized information sharing. Dr. Hunter suggested requiring community care providers to meet the same evidence-based care standards as VA providers, especially for mental health care. She explained that current systems only confirm a veteran attended an appointment without sharing detailed treatment plans, hindering coordination and comprehensive care.
Rep. Cherfilus-McCormick also asked for recommendations related to electronic medical records. Dr. Hunter acknowledged the VA's EHR system is flawed and expressed a desire to work with the Congresswoman’s office to develop better modernization strategies to enable seamless communication between VA and community care providers.
Rep. Cherfilus-McCormick then asked Ms. Newman about the impact of Medicaid cuts on home care agencies and how patients might be affected. Ms. Newman explained that her agency has little Medicaid exposure, but she confirmed that veterans have already lost access to VA services like homemaker and home health aid due to VA internal cuts. She agreed that patients are already being abandoned in some cases when services are withdrawn.
Rep. Maxine Dexter asked what data would be most compelling for advocating either community care or VA care. Dr. Hunter said that she prioritizes patient outcomes, stating that VA care generally leads to better outcomes because of its coordination model. She warned that shifting mandatory spending toward community care has reduced the VA’s ability to hire staff, creating a cycle of understaffing and lower morale that harms veterans’ experiences and outcomes. Rep. Dexter agreed and expressed interest in working with the Committee to gather more comprehensive data on access, quality, and timeliness of care across both systems.
Chairwoman Miller-Meeks asked whether the VA is responsible for setting care standards and training requirements for community care providers. Dr. Hunter acknowledged that the VA could be responsible but pointed to the lack of data to confirm the extent of this responsibility.
Chairwoman Miller-Meeks then asked Dr. Mobbs to confirm whether the VA can set such standards, and Dr. Mobbs affirmed that it can. She clarified that while VA providers receive training, it may not always be the appropriate type of training, particularly in mental health care, where veterans may prefer therapies not prioritized by the VA.
The Chairwoman asked Ms. Knight whether she received better care at the VA compared to community care. Ms. Knight responded that her experiences at the VA were poor, involving interrogative and invalidating interactions, even with a veteran provider. She claimed that community providers, including those who treat trauma-exposed populations like police and firefighters, can be well-qualified, and she advocated for giving veterans better information to choose their providers.
Chairwoman Miller-Meeks then asked Ms. Newman whether her agency has seen a decrease in community care referrals. Ms. Newman confirmed that there was a marked decrease in 2024, attributed to added layers of VA oversight aimed at reducing care authorizations. The Chairwoman concluded that despite some VA providers’ efforts to discourage community care, community care remains essential, especially when the VA system fails to meet veterans’ needs.
Dr. Hunter, in response to the Chairwoman, confirmed that the VA budget has continued to increase and that community care constitutes about 40% of all VA care, provided at approximately 25% of the cost of VA direct care. Chairwoman Miller-Meeks argued that the narrative that community care drains VA resources is inaccurate, given rising budgets and appropriations, including $75 billion more for VA medical services. She reiterated that veterans should have a choice, and as a veteran, she prefers community care.
Ranking Member Brownley said that while the VA budget has increased, the community care budget has grown at a faster rate. She shared VA data showing workforce gains in previous years, followed by a net loss of 10,000 employees between 2024 and 2025, which she warned could limit veterans' choices. The Ranking Member echoed the importance of balancing support for VA care and community care to prevent the deterioration of either option.
Chairwoman Miller-Meeks cited VA data indicating an annual 9% workforce attrition rate, equating to about 38,000 employees, and reaffirmed that veterans deserve choice in their care. She argued that community care exists because the VA system had failed to meet demand in critical areas like mental health and residential treatment.
SPECIAL TOPICS
🖤 Mental health & suicide:
Dr. Hunter claimed that VA direct care leads to better mental health outcomes, noting that veterans receiving community care for mental health have a 25% higher suicide rate than those in VA direct care. She highlighted the importance of patient-aligned care teams in coordinating comprehensive mental health treatment, stressing that community care providers are not required to report full treatment plans back to the VA.
Ms. Knight shared personal experiences of being retraumatized when discussing MST and receiving inadequate mental health support within the VA system.
Ms. Newman confirmed that veterans have lost access to VA homemaker and home health aid services, impacting care continuity, including mental health support.
Dr. Mobbs discussed that while VA mental health providers are trained in certain therapies, many veterans discontinue these treatments and desire other evidence-based options not prioritized by VA.
Chairwoman Miller-Meeks criticized the VA for failing to recognize residential mental health care under the MISSION Act, leading to long wait times for critical care.
Dr. Conaway and multiple members expressed concern about mental health care coordination gaps between the VA and community providers.
👀 Eye care:
Dr. Hunter shared a personal story of being diagnosed with ocular melanoma by a VA optometrist after a community care optometrist missed it. She credited the VA provider’s familiarity with military exposures for the life-saving diagnosis.
👨💻 IT issues:
Rep. Murphy and other members criticized the VA’s longstanding failures to modernize its electronic medical records system, saying that incomplete record sharing impairs care coordination between the VA and community care providers.
Dr. Hunter identified poor system interoperability as a barrier to integrating VA and community care records, contributing to gaps in treatment continuity.
Rep. Cherfilus-McCormick discussed the need for joint oversight on EHR improvements and invited collaboration with Dr. Hunter to improve the system.
🧠 Traumatic brain injury (TBI):
Ms. Knight referenced her personal experiences seeking care for TBI-related trauma, sharing that VA neurology appointments sometimes felt like interrogations rather than supportive consultations.
♀️ Women veterans:
Dr. Hunter and Ms. Knight criticized the VA for lacking sufficient MST-sensitive care pathways and failing to provide trauma-informed care consistently.
Dr. Mobbs emphasized that 70% of women veterans prefer female providers for women-specific care, and 50% prefer them even for general care.
Multiple witnesses and members highlighted that VA direct care often lacks adequate women’s health specialists, requiring referrals to community care.
Chairwoman Miller-Meeks and Ranking Member Brownley both discussed that women veterans may have no choice but to seek certain services, like maternity care, in the community due to VA limitations.
JOIN THE NIMITZ NETWORK!
Enjoying our updates? Don’t keep it to yourself — forward this email to friends or colleagues who’d love to stay informed. They can subscribe here to become part of our growing community.